Posterior Instability and Labral Tear
Introduction
Posterior instability occurs in only about 10% of all cases of shoulder instability. Although the most well-known type of instability involves outright dislocation, posterior instability may be subtler, often presenting with pain rather than dislocations.
While they are, indeed less common, I see them rather frequently in active sporty individuals. In this section, I have chosen to discuss the 2 topics together because their presentation and treatment are rather similar.
To learn more about posterior instability and labral tears, basic knowledge of the anatomy of the shoulder joint is necessary.
Anatomy of the Shoulder Joint
The shoulder joint is made up of 3 bones: the shoulder blade (scapula), the humeral head and the collar-bone (clavicle).

Movements around the shoulder involve 3 separate articulations: the glenohumeral joint, the acromioclavicular joint and the scapulothoracic articulation. When the arm is raised, the majority of movement occur at the glenohumeral joint and the scapulothoracic articulation.
The glenohumeral joint is a ball and socket joint, comprising the socket (the glenoid) and the ball (the humeral head). Both surfaces of the joint are covered with an extremely smooth and rubbery cartilage (known as articular cartilage). The smooth surfaces create a frictionless articulation when lubricated with a small amount of joint fluid.


The glenoid is really a rather shallow socket. In fact, a dish is probably a more accurate description! This, however, is a design which is intended to allow the shoulder joint to have great range of movement. Unfortunately, the price of big range of movement is stability. You can probably image that a big ball sitting on a shallow dish will fall off very easily.
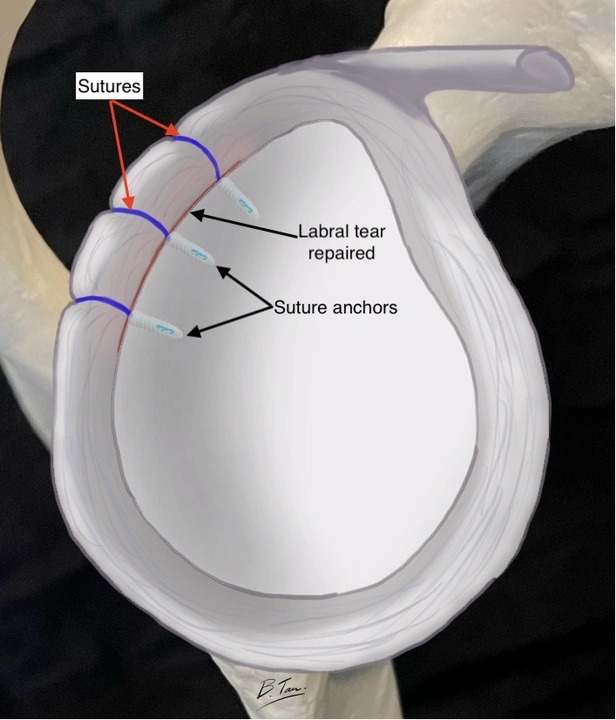
While that is true to a certain extent, the body has ways of preventing this from happening. A ring of cartilage attached to the rim of the glenoid helps to not only deepen the socket, but also serves as the attachment point of ligaments that help to hold the humeral head in place. This ring of cartilage is known as the labrum. The view of the glenoid seen end-on further demonstrates the labrum.
Note: Ligaments attaching the labrum and glenoid to the humeral head are not shown in order to allow readers to appreciate the importance of the labrum.

What is posterior instability?
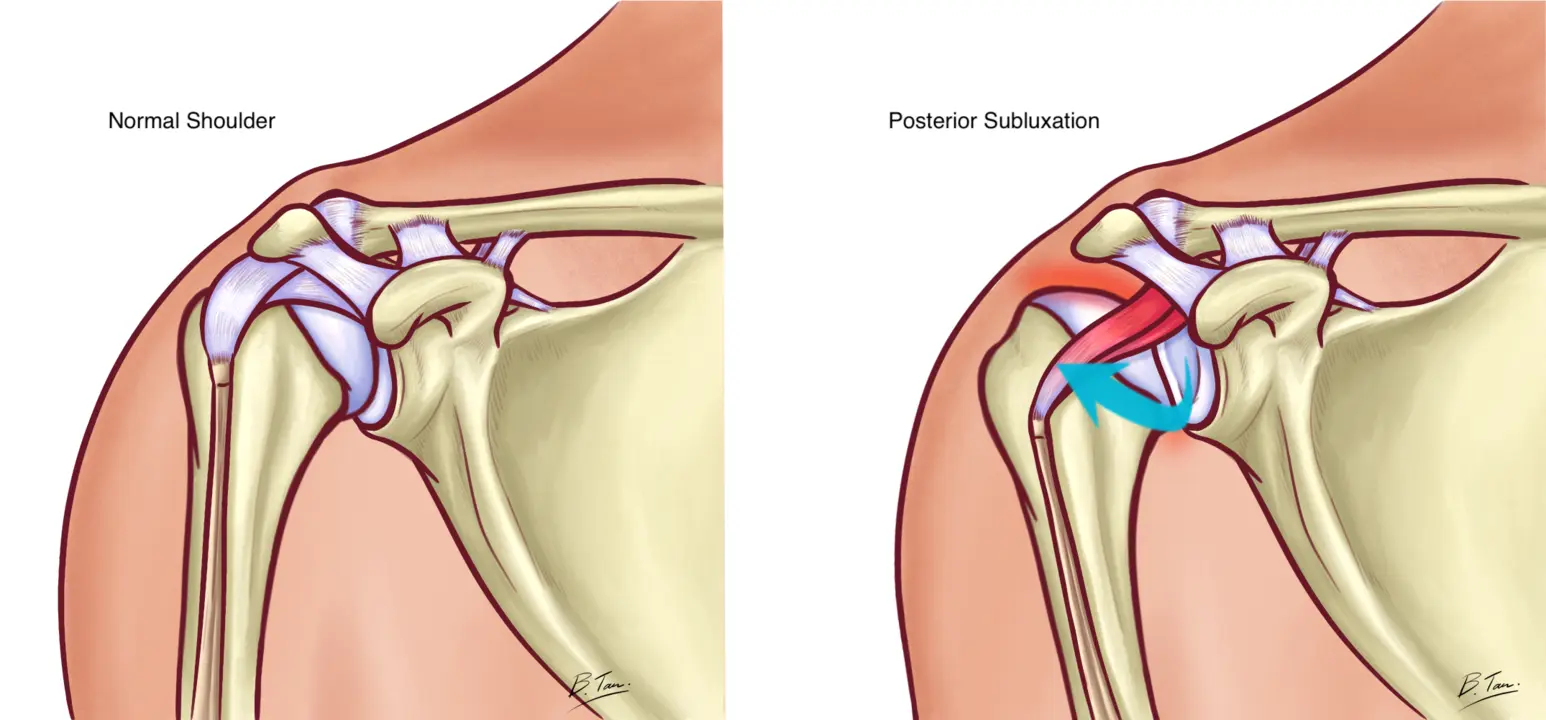
Posterior instability means that during some movements at the shoulder joint, the humeral head shifts backwards in relation to the glenoid.
In many cases, the slight shift does not result in a dislocation, but rather a subluxation. Meaning the shoulder joint does not completely pop out backwards but only comes out partially before snapping back in place.
This subluxation may be something that occurs all the time when patients lift their arms, or may be an acute event during an accident.
What is posterior labral tear?
Similar to the common anterior dislocation, the force of the humeral head sliding backwards may cause the labrum at the back of the glenoid to shear off the glenoid edge. While posterior labral tears can and do occur with violent forceful events like motorcycle accidents, they occur more commonly with repetitive movements like weight lifting, overhead movements like serving during tennis games, spiking a volleyball etc.
Who gets posterior instability or posterior labral tears?
Sports injuries are the leading cause of posterior instability/ tears. They are often seen in young active patients. Sports such as weight-lifting, baseball, tennis or volleyball etc are common causes of this injury. Any activity that involves posterior loading of the arm (like doing heavy bench presses) and forceful overhead movements can cause posterior labral tears to occur.
What symptoms do posterior instability or posterior labral tears cause?
The most common complain is pain. The pain is also typically experienced at the back of the deltoid region, and usually occurs only during and after sports. Similar to SLAP tears, most patients do not have much pain at all with activities of daily living. (Please refer the section on SLAP tears to learn more).
They can actually go about their lives absolutely pain free and that includes lifting heavy loads. However, they will get pain when they participate in sports that involve throwing like baseball, handball, dodgeball, water polo etc.
They will also have pain with sports that involve a lot of overhead movements like tennis, badminton, volleyball etc. Sometimes, patients may find that they pain is most bothersome when they first start playing.
It may then mellow down a little throughout the game, but they may get a sore shoulder that lasts for a few days after the game. Others may find that they are no longer able to serve or throw as hard as they used to.
Many will find that they are not able to perform some gym exercises like bench presses or dumbbell presses. Some patients may experience a clunking sensation midway through the movement whenever they try to lift their arms overhead.
What will the doctor do?
He will have a suspicion that you might have suffered a labral injury, after having heard your symptoms and your sporting activities. Examining your shoulder will help to further strengthen his suspicion but he will need to investigate further by way of an MRI scan in order to confirm the diagnosis.
Why do I need an elaborate MRI scan? How about an x-ray?
MRI scans are required to diagnose posterior labral tears. Other investigations are either woefully inaccurate or outright useless! MRI scans are not elaborate at all and are actually extremely commonly performed these days.
I have found that subtle posterior labral tears can be missed even by an MRI scan. As such, some doctors may prefer an invasive form of MRI scans known as MR arthrography. In an MR arthrography, the radiologist first injects a dye into the shoulder prior to performing the MRI scan. While an MR arthrography does increase the accuracy of the scan slightly. I do not routinely order MR arthrography despite their marginal higher sensitivity because I have had missed posterior labral tears with MR arthrography studies as well.
It is hence, very important, to see a doctor who is familiar with shoulders and shoulder surgery because a high index of suspicion is required to accurately make the diagnosis, based on the clinical presentation.
Will a shoulder with posterior instability become stable with time?
Unfortunately, this is not likely at all. In fact, if patients are athletes in whom their shoulder function is vitally important, waiting for the shoulder to “stabilize itself” is likely to be a frustrating exercise in futility.
Will the posterior tear heal by itself?
Unfortunately, again, posterior labral tears do not often heal by themselves. It is postulated that the presence of joint fluid tends to flush away chemical factors that the body produces to effect healing, hence interfering with the labrum’s ability to heal. At best, the tear remains as it is.
However, some patients find that the pain they had initially slowly abates and disappears with time! This is likely because the initial inflammation that the tear caused slowly resolves and the pain goes together with the inflammation. And if these patients are not high demand athletes, their level of activity may not irritate the shoulder so much and they then find that they are able to cope just fine.
How is posterior instability or posterior labral tears treated?
Patients usually only have 2 options:
1. Leave it alone and perhaps try a course of physiotherapy. It is unlikely that physiotherapy will “heal” the posterior instability or labral tear but it may improve the shoulder dynamics, hence improving function and reducing pain.
2. Stabilize the shoulder and repair the tear via surgery
What does posterior instability/ labral repair surgery entail?
The surgery is performed under general anaesthesia and is done via keyhole surgery (minimally invasive surgery). Stitches are passed through the torn labrum and securely fastened to the glenoid using small implants known as suture anchors.
There are endless types of suture anchors and most perform similarly. Which type of suture anchors to use ultimately depend on surgeon preference and familiarity. To know more about keyhole surgery, please read the section on Keyhole Surgery.

What is the success rate of the surgery?
Chances of success are excellent! In excess of 90%! However, this is only true if the right diagnosis is made.
As mentioned above, diagnosis of posterior instability and posterior labral tears may not be as straightforward as simply seeing the tear on the MRI scan. Also, because posterior labral repairs are not as common as anterior labral repairs (surgery done for the common anterior shoulder dislocation), the surgery could be technically challenging for surgeons who are not so familiar with shoulders.
As such, it is advisable to seek out a surgeon who is familiar with sports and shoulder surgery.
Will I be able to participate in sports after the surgery?
Absolutely. The aim of the surgery is to restore stability to your shoulder, not just during daily activities, but also during sports.
What should I do now?
If you have managed to get to this part of this long article, your shoulder must be bothering you significantly! Consult your family doctor or see an orthopaedic specialist and he/she should be able to advise you accordingly.


 ">
">

 Dr Bryan Tan
Dr Bryan Tan